Fifteen years ago, at a scientific meeting on Colorado State University’s Mountain Campus, a colleague asked immunologist Tony Schountz a question that was starting to percolate in the minds of infectious disease experts: “What do you know about bats?”
“Well, most are made of ash, but some are made of maple,” Schountz replied. He had played baseball in college; and, until then, his immunology studies had centered on hantaviruses, a family of infectious agents spread by deer mice and other rodents. In 2005, Schountz really did know more about wooden baseball bats than he knew about the world’s only flying mammals.
But the question proved prophetic. It came on the heels of a global outbreak of severe acute respiratory syndrome sparked in 2002 by a new coronavirus. The virus had not been earlier identified, much less as a cause of human disease. It was dubbed SARS-CoV.
As researchers later surmised, the SARS virus pulled off a rare feat enabled by the mixing and mingling of nature, animals, and man. The coronavirus apparently hopped from horseshoe bats in southern China, skipped to a wild catlike creature called the masked palm civet, jumped to people – with an assist from viral exchange at a live animal market outside Hong Kong – and then flared into an outbreak of respiratory disease passed from person to person. SARS spread through more than two dozen countries. It resulted in upward of 8,000 known infections and nearly 800 deaths. Sound familiar? That’s because SARS predated two other novel coronavirus contagions following an eerily similar route, in all likelihood starting with bats: an epidemic of Middle East respiratory syndrome in 2012 and the current COVID-19 pandemic. The virus that spawned today’s health and economic crisis is SARS-CoV-2.
More than 60 percent of communicable diseases in people have spilled over from animals, a category known as zoonotic disease. And 75 percent of new or emerging infectious diseases are zoonotic, the World Health Organization reports. That includes COVID-19.
These facts are well-known among those who study contagious disease. Even so, the SARS outbreak was a wakeup call for the scientific community, which earlier had regarded bats mainly for their ability to spread rabies. Knowledge about SARS grew more compelling alongside mounting evidence that fruit bats were the natural source, or reservoir hosts, of Ebolavirus. It was discovered in 1976 and identified as the spark for a storm of Ebola virus disease in Africa. After these outbreaks, researchers increasingly asked if bat colonies could serve as enormous vats for infectious pathogens that might cross species barriers to threaten human health – much as birds, rodents, nonhuman primates, and other creatures have hosted and transmitted disease across time. Consider plague, caused by the bacterium Yersinia pestis and spread by bloodsucking fleas from rats to people; the Black Death pestilence of the Middle Ages is known as the most lethal outbreak of infectious disease in recorded human history.
“Bats are amazing animals. They are very important to natural ecosystems, and we’ve learned they are reservoirs of innumerable viruses, some of which have emerged to become really significant pathogens in humans. It’s almost frightening the number of viruses bats can be infected with that cause no illness to them,” said Barry Beaty, a University Distinguished Professor Emeritus who is internationally known for research into severe human diseases spread by mosquitoes. Beaty co-founded CSU’s Arthropod-borne and Infectious Diseases Laboratory, known as AIDL, where Schountz conducts research.
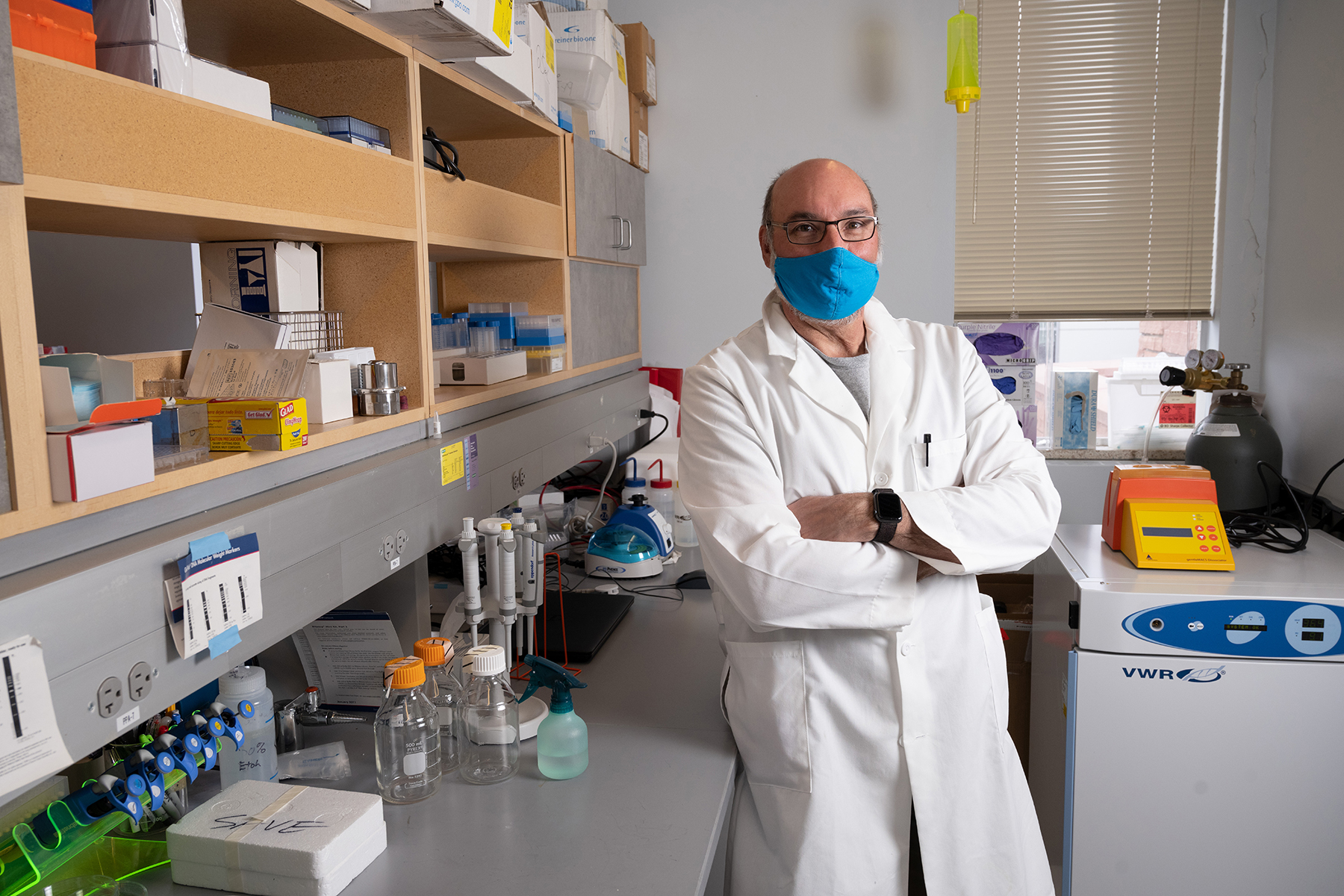
In recent years, Schountz has become Colorado State’s resident bat man. He is a foremost expert on the bat immune system and its uncanny ability to halt viral disease. The issue is central to understanding the new coronavirus pandemic – and to development of potential vaccines and treatments – because genomic analysis has identified horseshoe bats in China as the probable source of SARS-CoV-2.
Schountz is contributing to three federally funded studies tied to SARS-CoV-2, collaborating with partners at Colorado State University, the University of Pennsylvania, and Montana State University. He is conducting a vaccine study; investigating unique ways viruses influence host immunity; and examining bat immune response to environmental stressors that might prompt viruses to jump species.
To these projects, Schountz adds molecular analysis of disease avoidance in bats. He seeks insights that might help thwart infectious diseases in people. Put simply: Could the human immune system be medically encouraged to mimic that in bats? “We’re looking for clues about the workings of a successful immune response that does not cause damaging inflammation and disease,” said Schountz, an associate professor in CSU’s Department of Microbiology, Immunology, and Pathology. “We want to leverage that for vaccine candidates and new therapies.”
As scientists more and more have discovered, bats harbor many viruses. The microorganisms flow into and circulate among their hosts, like springtime snowmelt rushing into a reservoir. And viruses often breach the dam. They flush, or shed, into the natural environment and even move into other species, usually without causing harm.
But on rare occasions, pathogens spill over from bats to people and provoke bouts of virulent human disease, sometimes with other animals as intermediaries. Examples include rabies, Ebola, Marburg, and Nipah viruses, as well as the coronaviruses that sparked outbreaks of SARS, MERS, and, now, the dangerous respiratory disease COVID-19.
The movie Contagion, released in 2011 and noted for scientific realism, illustrated a transmission chain based on the real Nipah virus: bat, pig, index patient, epidemic. Nipah virus, naturally hosted by certain fruit bats, can cause acute respiratory infection and fatal encephalitis in people, making it a stark public health concern, according to the World Health Organization. As suggested in the film, a viral spillover might occur through contaminated blood, saliva, urine, feces, or tissue from a host species.
Andrew Dobson, who studies the ecology of infectious disease at Princeton University, described one viral path in a perspective titled “What Links Bats to Emerging Infectious Diseases?” published in 2005 in the influential journal Science. Bats, Dobson explained, nosh on fruits and insects and spit out uneaten bits and pieces. Those bits and pieces – speckled with virus particles in residual bat saliva – are easily encountered or ingested by other wild animals, livestock, or directly by people. “Knowing more about bats, and particularly more about bat ecology and immunology, is crucial if we are to develop new treatments and ways to control the viral diseases that are an increasing threat to humans,” Dobson wrote, presaging research to come.
COVID-19 presents a new round of questions about pathogen dynamics and emergence. Through sampling and genomic sequencing, scientists traced SARS-CoV-2 to a live-animal and seafood market in Wuhan, China. But they have not yet confirmed the site and circumstances of a spillover event. Some scientists ask whether an intermediate host, such as the illegally trafficked pangolin, or scaly anteater, might have served as a bridge to move the novel coronavirus from bats to people. Research recently published in journals, including Nature Medicine, has examined this possibility without clear answers. Yet the novel coronavirus closely resembles virus sampled from Rhinolophus affinis, a horseshoe bat species found in southern China. This means the bat is the likely reservoir host for the virus behind COVID-19, just as bats were behind several earlier malignancies.
But here’s the thing about bats: They don’t get sick.
“All of these viruses have bats as part of their biological cycles, but the bats have no signs of disease,” Schountz said, of deadly microorganisms harbored by bats. “We’re interested in how bats are able to host pathogens that are really significant in humans, but they don’t sicken bats at all.”
Schountz is among dozens of CSU researchers responding to the COVID-19 pandemic with new or quickly repurposed projects aimed at developing diagnostics, vaccines, and treatments to battle coronavirus disease. They join scientists around the globe in a race to combat the scourge.
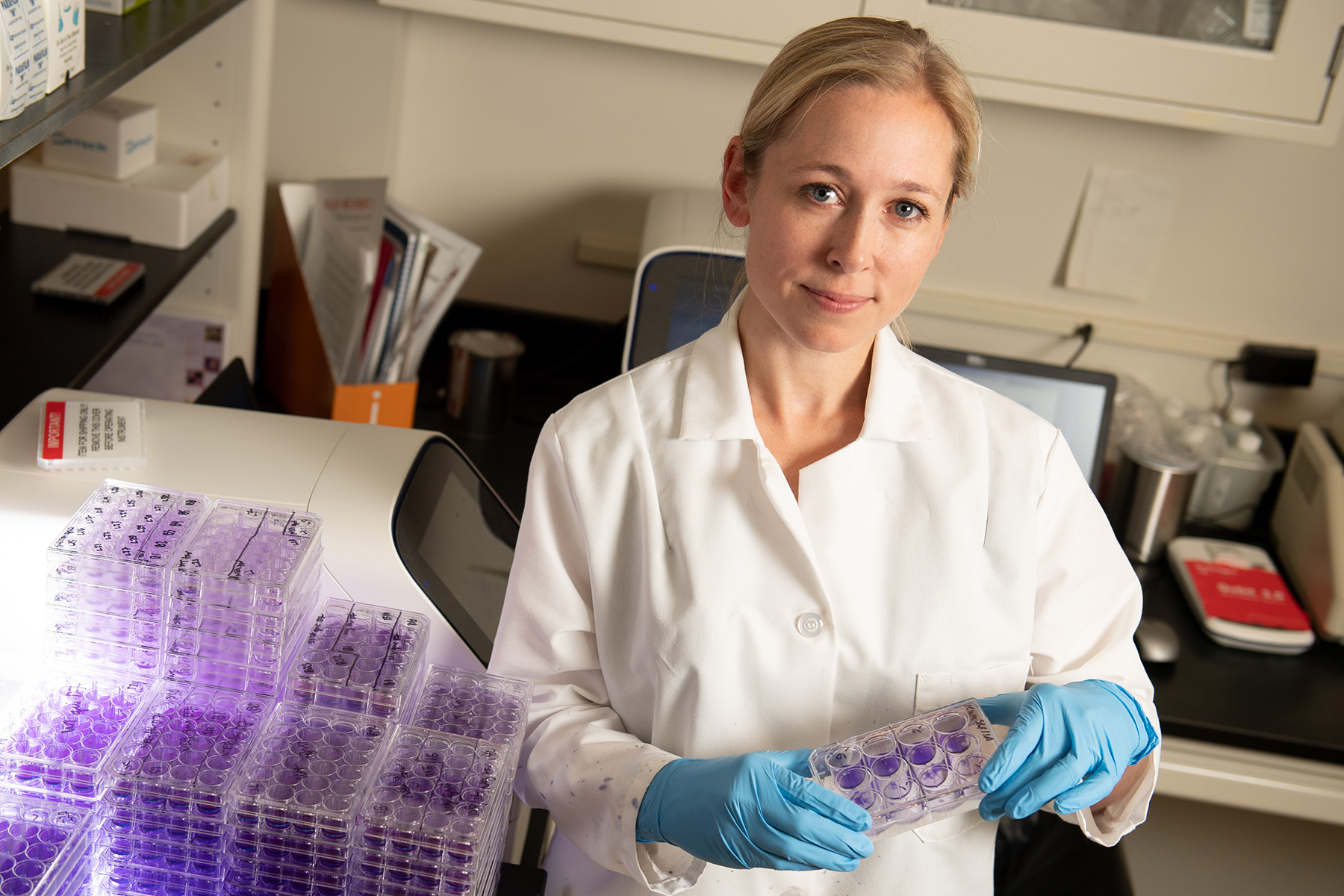
Rebekah Kading, one of Schountz’s colleagues in AIDL, is poised to start a five-year bat biosurveillance project, funded by the U.S. Department of Defense, in caves around Mount Elgon National Park in Uganda, a volcanic region on the border of Kenya. Kading and her team, partnering with local researchers, want to understand what viruses circulate among bat species in the region and how, in turn, those viruses move into the human population. They will collect blood and fecal samples from bats, examine the samples for viruses, and compare data to findings from human serum samples. They will even outfit bats with GPS devices – called “batpacks” – to track movement of the creatures and their microbes. Ultimately, the collaborative team hopes to identify health risks to people who live in the region and visit bat caves in and around the national park. “We’re expecting to find coronaviruses, which is a timely issue,” Kading said. “We’ll know a lot more about what pathogens are in the bats and how they’re circulating. It’s tying together the ecology of bats and infectious disease.”
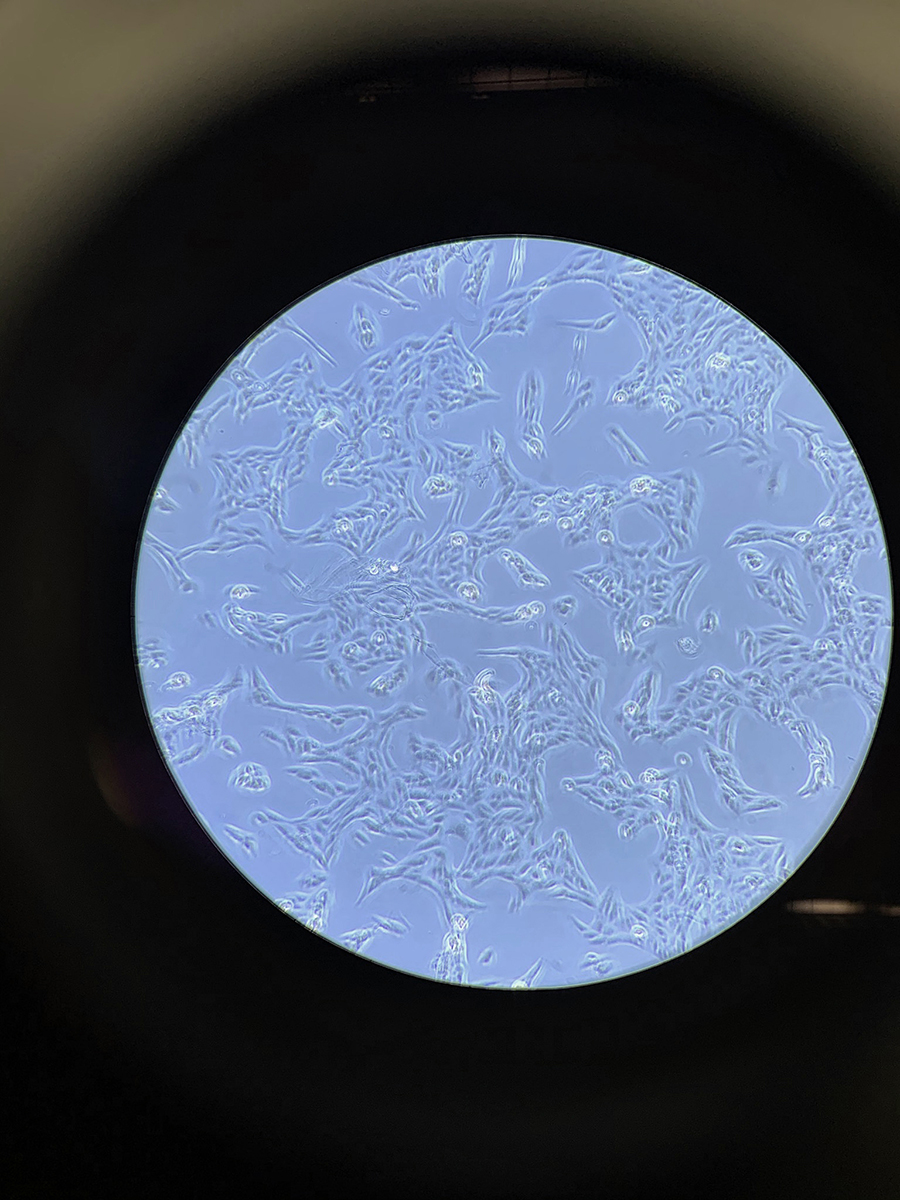
In many research projects, Schountz and his collaborators rely on a CSU breeding colony of about 100 Jamaican fruit bats. The bats are just 3 inches long, with distinctive leaf-like protrusions from their snouts. They live on a diet of fresh cantaloupe, watermelon, and bananas; females produce offspring every five months. The uncommon research colony provides a dependable supply of nasal, fecal, and tissue samples, imperative for sound scientific studies; the colony augments Schountz’s field studies in Trinidad and Grenada.
Virtually all of Schountz’s research examines the interaction of viruses and their reservoir hosts – a relationship he likens to a détente. The relaxation of wartime tension between invading virus and host immune system yields an equilibrium: The virus persistently replicates and sheds, as it is genetically programmed to do, while suppressing the host’s inflammatory response and the severe illness and death that could follow. The deal lets a virus keep on trucking, while the bat host flaps on its moonlit way, with little or no sign of disease.
The relationship is so unusual that Schountz and other scientists think viruses and bats have co-evolved over millions of years, through the continuous thrust of infection and parry of evasive immunity. Yet, viruses that churn in bats without producing illness have, at times, proven highly infectious when surfacing in the human population. In an article published in Frontiers in Immunology in 2014, Schountz and his co-authors hypothesized that evolutionary dynamics make some viruses more dangerous when they cross to animals with different defense mechanisms, including people.
Of course, bats are not completely impervious. They are susceptible to some diseases that dramatically impact their health and ecology, as Schountz noted in a commentary published in the journal Viruses. For instance, white nose syndrome, caused by a fungus, has killed millions of bats in North America, including some threatened and endangered species.
Yet their role as reservoir hosts of emerging viruses has put bats in the scientific spotlight.
“Tony is one of the great experts on viruses that persistently infect bats,” said Carol Blair, an esteemed professor emerita of virology who joined Colorado State in 1975. As the first female head of CSU’s Department of Microbiology, she urged teaching and research in infectious disease and, with Beaty, led formation of the Arthropod-borne and Infectious Diseases Laboratory; she still collaborates with its faculty. “It’s very important work,” Blair continued, referring to research into bat immunity. “I credit Tony for being one of the early ones to recognize that importance.”
His focus on bats began when Schountz was at the annual fall meeting of the Rocky Mountain Virology Association in 2005. He and a few colleagues gathered for beer and pretzels after a day of presentations. Their discussion turned to bats and viruses.
Three years before that, SARS had swept through Asia, Europe, North America, and South America, leading to critical cases of pneumonia, before aggressive public health measures helped halt the outbreak. The scientific community needed to know more about bats and their ability to host novel viruses that might jump to people and cause alarming outbreaks of infectious disease.
That’s when Charles Calisher, a CSU professor emeritus and a giant in virology, turned to Schountz and asked what he knew about bats. As the group chatted, a collaborator in the molecular biology program at the University of Colorado School of Medicine, Kathryn Holmes, suggested Calisher compile a list of viruses known to circulate in bats. It would be a good way to better gauge the potential for outbreaks of zoonotic diseases, she said.
“Why should I write a list? Why don’t you write a list?” Calisher objected.
But he was well-suited for the task, with decades of leadership in the field of arbovirology, the study of viruses transmitted by biting insects and other vectors, first at the Centers for Disease Control and Prevention and then in AIDL. So he relented. Calisher checked with far-flung researchers to assemble a list; the inventory ran to 66 viruses. That’s scant within thousands of described virus species, but revealing as a sign of bats as viral reservoirs. The effort grew into a review paper, with Calisher as lead author. He assigned sections to a population biologist, veterinarian, and two virologists; Schountz took the section on immunology.
“There’s nothing known,” Schountz said at one point.
“Then write questions,” Calisher said. “How come these viruses don’t wipe out entire colonies? These bats are snuggled up, breeding, urinating, and drooling on one another. There’s something weird about bats in terms of immunity.”
The paper, “Bats: Important Reservoir Hosts of Emerging Viruses,” lists viruses that consistently infect bats without inducing sickness. It also summarizes characteristics that make bats “exquisitely suitable hosts for viruses and other disease agents.” It’s a remarkable collection of attributes: the ability to fly, nocturnal activity, hibernation, roosting behavior marked by daytime torpor, evolutionary history, lifespan, valuable ecological functions, and breeding and feeding habits. In addition, the authors noted, bats make up more than 20 percent of all mammalian species and are found almost everywhere on the planet.
The editor of Clinical Microbiology Reviews, a journal of the American Society for Microbiology, snapped up the paper because it assembled important information earlier scattered or underappreciated.
“We’ll take it,” he told Calisher. “Bats are going to be a big deal.”
The review appeared in July 2006 and had an immediate impact, helping spur a wave of new research into bats and emergent infectious diseases. It has amassed 1,176 citations and counting, an impressive barometer of scientific influence. (The vast majority of published research papers are cited fewer than 10 times; those cited more than 1,000 times are rarities, the journal Nature has shown.)
“It activated this whole area of research into bats and their viruses,” Schountz said. For him, the paper has been a blueprint for years of subsequent investigations funded by the National Institutes of Health and the Department of Defense, among other top granting agencies.
Indeed, knowledge generated during the past 15 years about bats and infectious disease has been essential to understanding and responding to the COVID-19 pandemic.
Contributing such knowledge was exactly the plan when Beaty, Blair, and fellow faculty members formed AIDL in 1987. The group, based on the CSU Foothills Campus, was well-aligned with the international research agenda in its hunt for knowledge and innovations to control zoonotic diseases that often hit developing nations hardest, yet, as COVID-19 demonstrates, have zero concern for political boundaries.

“Good Lord, it was euphoria in the ’60s and ’70s, when everyone thought vaccines of the time were going to solve all these problems. In the end, that was wishful thinking,” Beaty recalled. “Our group always knew other zoonotic diseases were going to be important and emerging. Unfortunately, this is a growth industry.” Beaty helped lead a project for the Institute of Medicine, one of the authoritative National Academies, that resulted in a seminal research report published in 2003 and titled Microbial Threats to Health: Emergence, Detection, and Response.
From the start, AIDL specialized in serious pathogens spread by arthropods, including mosquitoes, fleas, and ticks. Think chikungunya, dengue fever, malaria, tularemia, yellow fever, and diseases caused by West Nile and Zika viruses, among others. The group also has discovered details about hantavirus ecology in rodents. Investigators have partnered with CSU veterinary colleagues – a key resource in studying zoonoses – and with those at local branches of the Centers for Disease Control and Prevention and National Wildlife Research Center, also on the Foothills Campus. Through such collaborations, AIDL helped establish the field of vector biology to shed light on interactions between pathogens and their conductors; the roles of rodents and bats are part of the broader puzzle.
AIDL faculty also have led national research training programs and have attracted grants from the largest federal funding agencies. These include $21 million from the National Institutes of Health to help build the Rocky Mountain Regional Biocontainment Laboratory, which provides expansive biosecure research space and houses a national Center of Excellence for Biodefense and Emerging Infectious Diseases, linked to similar centers around the country; the building’s final phase opened in 2008.
AIDL remains an indispensable part of the university’s teaching and research in infectious disease and is a cornerstone of the nexus on Foothills Campus. It fits under the umbrella of CSU’s Infectious Disease Research and Response Network, designated as a university Program of Research and Scholarly Excellence. Other groups in the cross-campus network include the Mycobacteria Research Laboratories, which study tuberculosis and leprosy; the Prion Research Center, which examines pathogens that cause chronic wasting disease, mad cow disease, and others with striking similarities to human neurodegenerative diseases; and the Veterinary Diagnostic Laboratories, which provide front-line surveillance and testing of zoonotic disease in animals. Rounding out these teams is the Infectious Disease Research Center, which often leads projects in partnership with government agencies and private industry. The center runs a state-of-the-art facility, called BioMARC, that develops and manufactures vaccines, diagnostic tools, testing reagents, and therapeutic drugs and devices.
This ecosystem gives CSU an edge in tackling infectious disease, said Ray Goodrich, a biotechnology investigator and executive director of the Infectious Disease Research Center. In fact, he noted, specialists across campus are pursuing COVID-19 solutions. These efforts include vaccine studies, coronavirus surveillance projects, analysis of antiviral drugs, and testing of personal protective equipment for health care workers.
“We have the people, the knowledge, and the facilities required for infectious disease research,” Goodrich said. He is evaluating a vaccine candidate that would use ultraviolet light and vitamin B2 to stop coronavirus replication while maintaining viral components that prompt human immune response. It is one of four COVID-19 vaccine development projects underway at the University. “The assets at CSU have allowed us to mobilize very quickly and bring some incredible talent to bear on the biggest event of our time affecting human health,” Goodrich said.
There is plenty of work ahead for Schountz and others in the Arthropod-borne and Infectious Diseases Laboratory. A new research facility will soon boost this work: The Center for Vector-Borne Diseases is under construction on the CSU Foothills Campus, with an anticipated opening late this year. The $23 million building encompasses about 40,000 square feet of new offices, biosecure laboratory space, and insectaries. It will bring together about 90 faculty members, research associates, students, and staff; they represent fields including virology, bacteriology, immunology, and computational biology. These are among the interconnected disciplines needed for new insights into the emergence and spread of disease – and possible paths for prevention and cures.
“I’m extremely excited about it,” said Blair, the retired professor who helped form AIDL. “If any good comes out of this devastating pandemic, I hope it’s the realization that we need to continue investing in funding for infectious disease research. This is an unusual pandemic, but it won’t be the last.”





